1. General Message
A well trained and committed group of us continues to dig deeply into past events at CDHB. We still feel that the money handed over recently by the Government was a smoke screen and a big con, just before the election. The Government could have stood back and waited for the CDHB to be unable to pay its bills. Or it could do the proper thing, and pay over new equity. It chose the latter.
Here’s some feedback on how the con about the funding was perceived. I had an email from within the medical system last week (they are rolling in!) and they said:
I was speaking with a CDHB clinician recently who stated they were relieved the planned deficit had been forgiven. Smart people, but commercially naïve!
The fact the announced equity injection figure ($180m) is the same amount as the 21/22 projected deficit ($180m) suggests a cynical plot to confuse and dupe the concerned clinicians and public.
However, the key issue is that there is still a Crown Monitor in place. There is still the Board which caused 7 of 11 of the Leadership team to resign. The incoming Government must remove both the Crown Monitor and the Board. Otherwise the rot which is in place right now will break up most of the gains of the last 11 years.
We had a rather annoyed Facebook posting from Andrew Dickerson last week about my calling for the Board to be replaced. I know he and Jo Kane have been brave and supported the former executive. However, the Government has been hoodwinked by Treasury and Ministry of Health into believing that nothing good was being done by the old executive. They will not leave, on any future Board, some who they think have been part of the problem, no matter how much we, members of the public, agree with those few with courage. They are more likely to leave John Hansen and his acolytes in place, and sack Andrew and Jo. So Andrew, sorry, all Board members should go and we should start again. Before too much more damage is done.
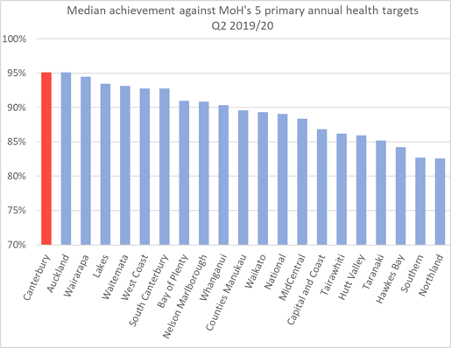
2. Here’s how the CDHB performed when measured against others:
This graph demonstrates just how good the CDHB really was, despite what the MOH say about them. Results are results.
3. Ian Powell continues to write analysing DHB’s and health issues:
This week Ian has written a summary of where DHB’s are financially. Here’s some quotes from this paper:
- DHBs deficits have been increasing exponentially since around 2015. In the financial year ended 30 June 2020 19, out of 20 DHBs recorded deficits.
- in relative terms, DHBs have been significantly underfunded since 2009.
- The first two budgets of the current government slightly improved funding in relative terms while there is a discernible improvement in funding for this financial year although this is likely only to alleviate rather than remove many deficits in 2020-21.
- DHB health services are demand driven. There is not a tap that DHBs can turn off.
- it is the politically and bureaucratically maligned CDHB that has been most successful in addressing acute admissions demand by bending the curve through its approach to clinical leadership and engagement between community and hospital care.
- There is a third driver which affects those DHBs who are undertaking major capital works (hospital and other facility construction). These lead to big financial costs for DHBs through depreciation and capital charges. Major rebuilds are project managed by the Health Ministry despite it having less expertise in this area than DHBs.
- CDHB had to cope with the additional factors associated with the earthquake including depreciation, capital charges, major delays in rebuilding (which was project managed by the Health Ministry) and having to outsource 10 operating theatres to the private sector. These all contributed massively to costs. Such was the relative cost effectiveness of CDHB’s leadership culture that had there been no earthquake then, unlike the other 18 DHBs with deficits, it may not have had a deficit (or at worst a relatively small one).
Getting and staying out of deficits
The easiest way to reduce DHB operational deficits would be to increase government funding to a level that would meet these largely anticipated costs. But there are three other actions required:
- a new funding mechanism needs to be developed to assist those DHBs confronted with natural disasters such as the Christchurch earthquake. Former Health Minister Tony Ryall’s decision to ignore advice to do this after the 2010 earthquake was a fatal mistake that must never be repeated.
(ii) we need a different method of funding major capital works. Funding them out of annual operational costs is too big an ask of DHBs. DHB chief finance officers collectively would be an excellent place to start considering this challenge. At the very least the capital charge should be binned consistent with the Auditor-General’s previous advice.
(iii) comprehensive clinical leadership distributed at all practical levels in DHBs needs to be actively encouraged. This was a priority of former health ministers Annette King, David Cunliffe and Tony Ryall but since then government interest has been non-existent. This subsequent disinterest is both retrogressive and fiscally irresponsible.
Here is Ian Powell’s paper:
Leave a Reply